 Dr Laura Johnson, Senior Lecturer in the Centre for Exercise, Nutrition and Health Sciences, discusses her new paper in which she assesses the impact of dietary patterns on obesity and how modelling may help influence change in both personal habits and public policy.
Dr Laura Johnson, Senior Lecturer in the Centre for Exercise, Nutrition and Health Sciences, discusses her new paper in which she assesses the impact of dietary patterns on obesity and how modelling may help influence change in both personal habits and public policy.
No single food or nutrient is to blame for obesity. There so many routes from diet to overeating and weight gain, and in real life foods and nutrients aren’t eaten on their own. So, it’s misleading to look at foods that way in research, it’s the overall balance of diet that matters.
I realised this a while ago when I used detailed records of food intake from children age 5 and 7 in the ALSPAC cohort to generate an overall diet score that predicted obesity later on. I thought that eating more fat, less fibre, and having a more energy dense diet (more calories in each bite) would all feature in a diet that fuels obesity (or an ‘obesogenic’ diet). I used reduced rank regression or RRR (a pimped up version of factor analysis, see excellent explanation by Andy Field here) to find the best combination of foods to capture differences in the fat, fibre and energy density of the children’s diets. RRR generates a score based on what you eat. It’s calculated by adding up the intake (grams/day) of 42 groups of foods that are weighted for importance and a higher score means your diet is more obesogenic. I showed that children with the highest pattern score at age 7 were 4 times more likely to have too much fat by the time they were 9 years old (other researchers have since seen similar associations in adolescence and adulthood).
A pretty strong result, right? But, what use is a score made up of 42 foods? Isn’t it too complicated to ever be the basis for changing behaviour? I don’t think so, not if we use computers to deal with the complex calculations. All we need to know is what foods have been eaten (by individuals or populations) and then the obesogenic score can be computed automatically. We would then have a single score indicating whether the overall balance of your diet (or the Nation’s diet if thinking in policy terms) is more or less obesogenic. A total diet score would be better than current measures which only focus on fruits and vegetables or sugar-sweetened drinks, which let’s be honest, no one believes are going to solve the obesity epidemic on their own!
In our latest paper we asked “Do the same foods make up an obesogenic diet regardless of whether you are young or old, boy or girl, rich or poor?” (Because the ALSPAC score might only matter to children living in Bristol in the late ‘90s) “Who in the UK has a more obesogenic diet?” (Because those people need the most help to change) and “Are diets getting more obesogenic over time?” (Because that might suggest national obesity policy isn’t working).
To find some answers we used diet diaries from nearly 10,000 adults and children taking part in the UK National Diet and Nutrition Survey between 2008 and 2014. We repeated the RRR in different groups and found it was remarkably stable – the same foods came out as most important to an obesogenic diet over and over again. So, we can feel confident that the obesogenic pattern score and that way foods are weighted by importance reflects the way everyone eats in the UK today. The most and least obesogenic foods we found were (sized and in order of importance):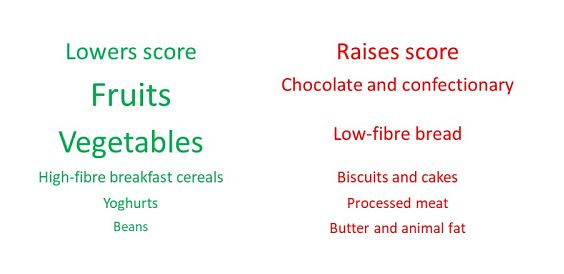
In terms of whose diets are most imbalanced we found massive social gradients with those in manual jobs and households earning less than £15,000/year having the most obesogenic diets, which mirrors social inequalities in obesity prevalence. Among children, diets became more obesogenic between 2011 and 2014. Among adults a more obesogenic diet went hand in hand with more time spent watching shows on TV/Laptops/Tablets, less physical activity, and eating takeaways more frequently.
All these trends are a starting point for targeting and testing interventions designed to make small changes across a range of foods to shift the balance of diet. By using our score, it could be possible to gauge how multiple changes to policy or what we eat adds up to a less obesogenic diet and with luck prevent obesity in future.


